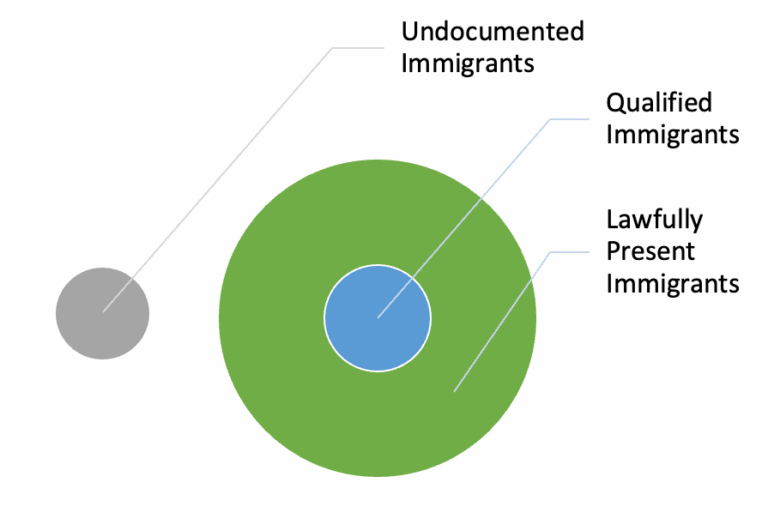
The proposed changes in the House-passed reconciliation bill have sparked confusion and concern about immigrant eligibility and enrollment in Medicaid and the Children’s Health Insurance Program (CHIP). Under current law, undocumented immigrants are not eligible for comprehensive coverage through these programs, and many lawful immigrants also face restrictions. To qualify for Medicaid or CHIP, noncitizens must meet typical eligibility requirements and have a specified ‘qualified status’ for a certain period.
Current Challenges and State Efforts
Many immigrants lack coverage options, leading to poor health and economic outcomes, particularly for children and pregnant women. In response, states have developed various solutions to provide essential health care to immigrant populations, often prioritizing these vulnerable groups. However, the House Republican bill includes a provision that would penalize states for providing health coverage to noncitizens by reducing their Medicaid expansion funding.
Details of the Proposed Penalty
The original bill text targeted states that cover undocumented immigrants with state-only funds. However, subsequent changes broadened the penalty to include states that provide coverage to lawfully residing children and pregnant women under certain programs. The current bill text would penalize states that cover ‘an alien who is not a qualified alien and is not a child or pregnant woman who is lawfully residing in the United States and receiving medical assistance pursuant to section 1903(v)(4).’
Impact on Various Immigrant Groups
The bill’s provisions would affect several populations currently covered by state programs:
- Immigrant children in separate CHIP programs covered under the ICHIA option
- Immigrant pregnant women covered through separate CHIP programs
- Additional qualified individuals during the five-year waiting period
- Other immigrants, including lawfully present and undocumented immigrants
- Lawfully present and undocumented pregnant women with postpartum coverage funded through CHIP Health Services Initiatives
- Certain immigrants admitted due to urgent humanitarian reasons or significant public benefit
Consequences of the Proposed Changes
The penalties would force states to drop coverage for these groups or face significant reductions in federal Medicaid expansion funding. This creates an unfair situation where expansion states that cover immigrant populations would be penalized, while non-expansion states offering similar coverage would not face penalties. The result could be a loss of coverage for hundreds of thousands of individuals, potentially harming their health and economic well-being.

Critics argue that the bill’s provisions overstep by penalizing states for using their own funds to provide coverage to immigrant populations not eligible for federal Medicaid funding. The changes could have far-reaching consequences for the health and well-being of vulnerable populations, including lawfully present children and pregnant women, as well as individuals covered by state-specific programs.